“The D-EYE Retinal Imaging System efficiently captures quality photos of the posterior pole in situations where standard fundus photography was impractical” – Doctor Pihlblad
D-EYE Retinal Screening SystemPresented by Ross Eye Institute at the American Association of Pediatric Ophthalmology and Strabismus Conference (AAPOS)
PADOVA, Italy and PASADENA, Calif. – May 10, 2016– Matthew S. Pihlblad, MD and Steven G. Stockslager, MD, physicians from the Ross Eye Institute, Department of Ophthalmology, The State University of New York at Buffalo incorporated the D-EYE Smartphone Retinal Imaging System into a recent study to determine if the system was a beneficial alternative for fundus imaging in the pediatric population. The results of the study were presented to the American Association of Pediatric Ophthalmology (AAPOS) at the organization’s annual conference.
During the course of the study, D-EYE was used with an iPhone 6 to obtain retinal images of pediatric patients in both outpatient and inpatient settings, on dilated and undilated eyes. The physicians found that D-EYE was especially helpful in aiding exams in remote settings and with immobile patients due to its compact and lightweight design.
“Our aim was to capture quality images of a variety of fundus pathologies to demonstrate the portability and efficacy of this relatively new device,” stated Dr. Steven Stockslager of Ross Eye Institute and co-author of the study.
The smartphone-based digital ophthalmoscope, D-EYE, easily attaches to iOS and Android devices via a specially designed, lightweight bumper. D-EYE utilizes the phone’s camera lens and LED light source, which is off-axis from the camera aperture, to illuminate the interior of the eye for examination, resulting in no corneal glare.
D-EYE uses the principle of direct ophthalmology. When the pupil is dilated, the device captures a field of view of approximately 20 degrees in a single fundus image at a distance of 1 cm from the patient’s eye. When examining an undilated eye, the field of view is approximately 5-8 degrees. Videos are the preferred method of acquisition as they allow the user to angle the lens to see more structure of the retina. Users pan the retina, starting from the posterior pole, and then move to the upper, nasal, inferior, and nasal peripheral retina to the equator. Color digital images and videos of the retina can be obtained, encompassing the posterior pole, including the macula, optic disc, and (limited by the field of view) towards the peripheral retina.
“The captured images were helpful for documentation, follow-up, and discussion of complex cases with colleagues and patients alike,” stated Dr. Matthew S. Pihlblad, Clinical Assistant Professor practicing pediatric ophthalmology and strabismus at the Ross Eye Institute.
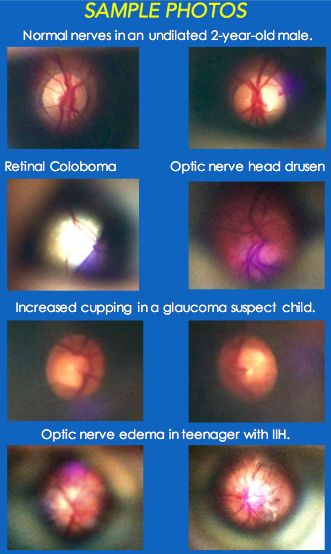
The study concluded that a portable system like the D Eye Ophthalmoscope has a “niche in situations when and where conventional fundus photography is not an option.” Doctors Pihlblad and Stockslager concluded that the D Eye Portable Retinal Imaging System can “document a diffuse range of pathology” including “optic nerve, hypoplasia/cupping/pallor, colobomas, optic nerve pits, drusen, neuroretinitis,” and more. Further, they concluded, “D-EYE may also be clinically useful for non-ophthalmologists (general practitioners, pediatricians, emergency physicians, neurologists, etc.) due to the significant potential for telemedicine consultation.”
About the Authors
Dr. Matthew S. Pihlblad is a Clinical Assistant Professor practicing pediatric ophthalmology and strabismus at the Ross Eye Institute, University at Buffalo (UB). He completed his ophthalmology residency at UB
, then Pediatric and Strabismus fellows hip at the Jules Stein Eye Institute, UCLA before returning to Buffalo.
Dr. Steven G. Stockslager is a PGY II resident at the Ross Eye Institute, SUNY Buffalo. He earned his MD from New York Medical College in 2009 prior to serving in the US Navy for 5 years as an Undersea Medical Officer in Charleston, SC. He will be the Chief Resident for the 2016-2017 academic year and plans to pursue a cornea fellowship after graduation.







